University of Minnesota researchers are on a mission to treat diabetes, and they’ve enlisted a few trillion microscopic helpers.
In place of drugs or surgery, a team of researchers is studying how to improve diabetes patients’ insulin sensitivity by introducing trillions of beneficial bacteria into their intestines. Researchers believe this unusual approach, conducted through a fecal microbiota transplant, could improve how the body regulates blood sugar, the central problem in diabetics. The project is part of MnDRIVE (Minnesota’s Discovery, Research and InnoVation Economy), a $36 million biennial investment by the state that aims to solve grand challenges. As a part of MnDRIVE’s Transdisciplinary Research Program, the project will bridge multiple fields of research and bring together experts from across the U to work on the same clinical trial.
Patients with diabetes have too much glucose in their blood, which leads to a host of serious health problems, from heart disease to obesity. Dr. Alexander Khoruts, a gastroenterologist at the U of M and lead principal investigator on the project, said the right balance of bacteria has the potential to improve the body’s energy metabolism, in part by enhancing insulin function. Insulin drives glucose from blood into cells of the body.
“If we can improve insulin sensitivity, we will correct the central metabolic problem responsible for diabetes,” Khoruts said. “Diabetes is one of the main complications of metabolic syndrome, which is also associated with obesity, high blood pressure and liver disease. If we improve insulin sensitivity, we hope some of the other problems may also get better.”
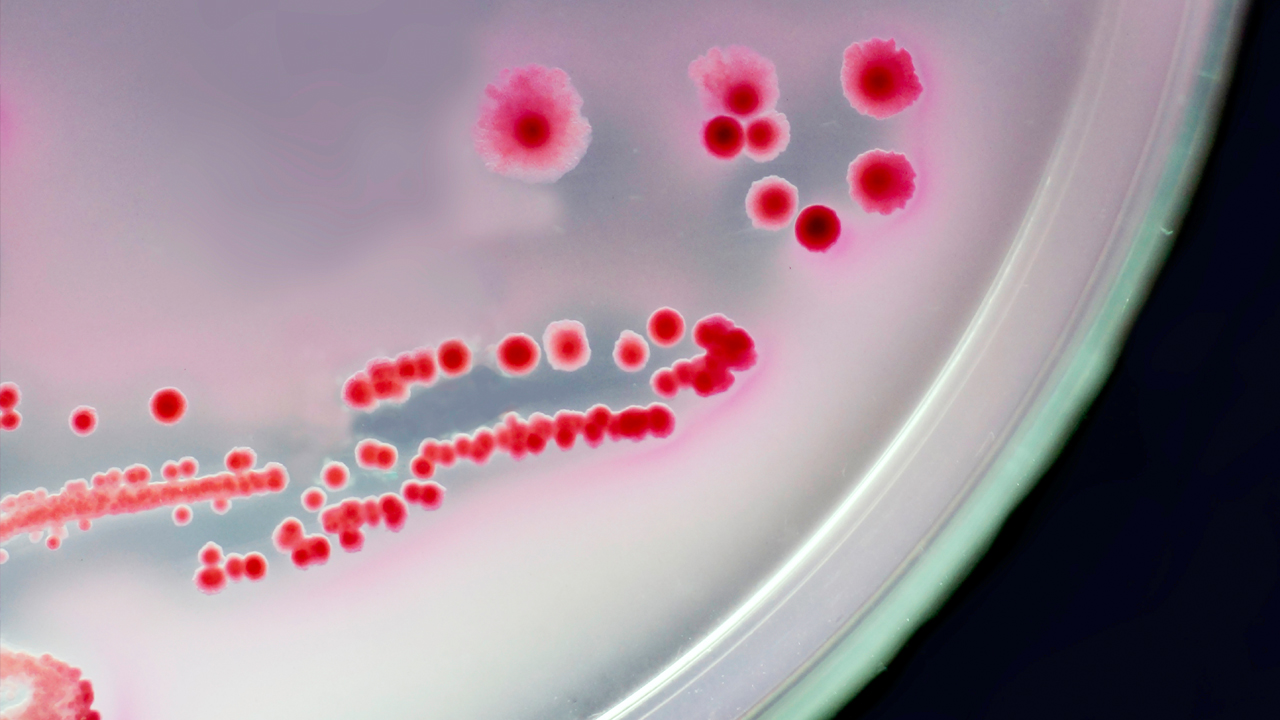
To understand the composition of microbes present before and after the transplant, Khoruts is working with Michael Sadowsky, Ph.D., director of the U’s BioTechnology Institute. As a microbial ecologist, Sadowsky studies the complex science of how microbes interact in their environment. People who are diabetic or obese tend to have a less diverse microbiome – or microbial community – in their gut. In turn, they are less able to produce important short-chain fatty acids, which may regulate many functions in the body, including appetite, glucose production, metabolic rate and the immune system. Khoruts and Sadowsky believe that a more diverse microbial gut community should be able to produce more short-chain fatty acids that will have a number of beneficial effects for the patients.
Feeding the problem
How do people lose a healthy balance of bacteria in the first place? Khoruts said one of the main culprits is antibiotics. Widely used across the globe, antibiotics suppress many bacteria in the gut, often disrupting the rich microbial communities that co-evolved with their human hosts for millions of years. In fact, on average, gut microbial communities in our society are less diverse than those found in more ancestral cultures. With the balance of bacterial species thrown off, some types of microorganisms may actually become more harmful and prey on others or attack the lining of the intestine. Over time, the widespread use of antibiotics across the world may have caused the human gut to have less microbial diversity, creating an environment ripe for problems.
The other main contributor to the problem is energy-rich, processed foods. Products high in sugar or high-fructose corn syrup, refined grains and fast food are digested earlier on in the small intestine, leaving little food for bacteria that are located at the end of the digestive tract in the colon. Starving bacteria may send signals back to the brain, telling the person to eat more. However, in our society that person may turn right back to the same processed foods that are detrimental to health and do not satisfy the hungry bacteria. This leads to a vicious cycle resulting in obesity, metabolic syndrome and diabetes.
Replacing bad bacteria
The researchers’ approach to treating diabetes builds off the success of Khoruts and Sadowsky’s first “personal bioremediation” project together. The two teamed up in 2009 to take on the potentially fatal Clostridium difficile, a type of infectious bacteria that releases toxins and damages the lining of the intestines. This infection is typically triggered by antibiotics. Normal gut microbial communities can keep C. difficile in check, but this protective function is lost when these microbial communities are disrupted. When C. difficile infection is treated with more antibiotics, the problem becomes worse. Therefore, they turned to the largely overlooked practice, first documented some 1,700 years ago, of using a fecal transplant to correct a person’s microbiome. The treatment proved spectacularly successful, able to cure approximately 98 percent of patients that failed all other standard therapies.
“We’ve taken what we learned in the lab and used this knowledge to improve patients’ health,” Sadowsky said. “Personal bioremediation, transferring a healthy individual’s microbes to heal another’s imbalance, opens new doors that could potentially result not just in deeper scientific understanding, but lasting remedies to a wide range of serious health problems.”
Clinical trial
Now, with their sights set on diabetes and experts from a variety of disciplines working alongside them, Khoruts and Sadowsky are preparing to begin a clinical trial in early 2015 that focuses on patients with pre-diabetes – those who have blood sugar levels that are higher than normal but too low to be type 2 diabetes.
To help ensure that all subjects will have the right food with potential to produce short-chain fatty acids, Douglas Mashek, Ph.D., a Department of Food Science and Nutrition professor and a specialist in the role of fatty acids in energy metabolism, will provide a specific diet to all participants in this trial. The subjects will spend two weeks on the fixed diet before taking antibiotics to prepare them for the fecal microbiota transplant. Then, one group will receive their own microbes back, while the other will receive microbes from selected outside donors specifically chosen as having normal blood sugar levels and good microbial diversity. Drs. Lisa Chow and Elizabeth Seaquist, endocrinologists from the Department of Medicine will directly measure insulin sensitivity of the participants before and after the intervention.
Before and after the transplants, Kelvin Lim, Ph.D., will scan patients’ brains while showing them pictures of food, recording the brain response triggered by microbes in the gut. Lim, a professor with the U’s Department of Psychiatry, will use the imaging to help Khoruts and Sadowsky better understand how microbial balance affects communication between the brain and gut – signals that scientists are only beginning to investigate, but that could give critical insight to the eating behaviors of patients at risk for diabetes. The team, which also includes David Bernlohr, Ph.D, from the Department of Biochemistry, Molecular Biology and Biophysics, will conduct exploratory studies to identify the molecules involved in these signals.
When the study is finished, the results will inform trials for other diseases that could benefit from this form of therapy. We may learn why diets by themselves may not be quite sufficient without the right microbes in place. Ultimately, this work should help development of new types of therapies that benefit the relationship we have with our own microbes and lead to better health.
“If the study is successful the impact will be huge,” Khoruts said. “It can affect how society views obesity and related problems and how to take steps to treat the problem in a more comprehensive way.”