
Rural Minnesotans are losing access to obstetric care, with recent closures in Fosston and New Prague. Birthing people in New Prague will now have to travel more than an hour away for service. The Fosston hospital is the nearest to the White Earth Indian Reservation, which is especially striking as Indigenous people are seven times more likely than white people to die around the time of childbirth in Minnesota.
This trend is not unique to Minnesota; it’s happening across the country, and the UMN Rural Health Research Center (RHRC) has been conducting research on rural maternity care for more than a decade. This trend of continued obstetric closures is significant, but now decision makers have a better sense of the potential consequences due to research conducted by the RHRC, whose research was extensively cited in recent public hearings about these two closures.
Rural People Know What’s Happening in Their Communities
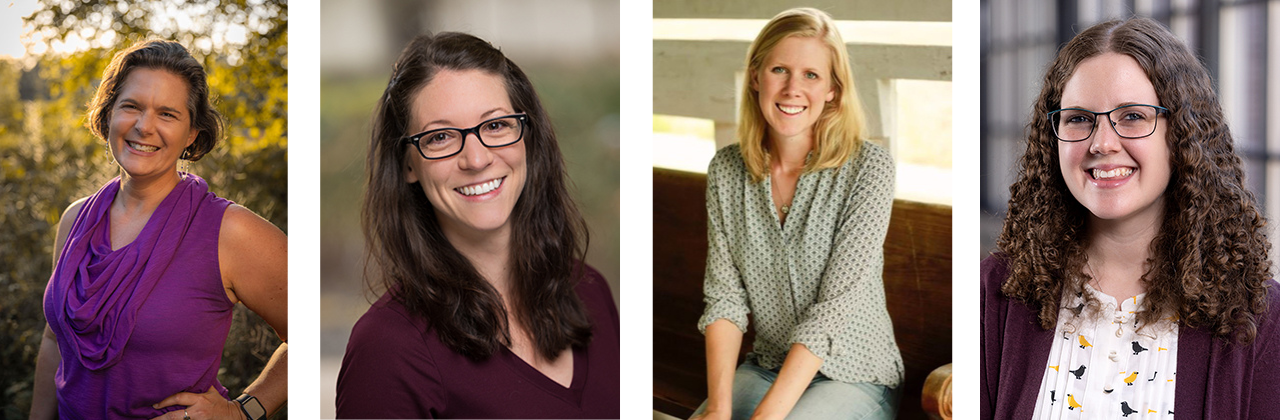
RHRC researchers look at access to and quality of care across the lifespan in rural communities, with deep expertise in aging, elder care, and end-of-life care as well as pregnancy, childbirth, and postpartum. The center conducts policy-relevant research and implements programs that improve the lives of rural residents by advancing equity and enhancing the quality of rural communities. They also pay attention to the issues rural residents themselves are noticing.

“Rural people know what’s happening in their communities, and we, as rural health researchers, should follow their leads,” said RHRC Director Katy Backes Kozhimannil. “Our best and most impactful work is when we are answering the questions that rural families have about their own lives then delivering those answers and their perspectives to policy makers and decision makers.”
More than Half of Rural Communities Lack Obstetric Care
The RHRC is also the only academic team in the nation extensively documenting obstetric closures. This is not an easy feat as there is no national data set of hospital services. To develop a comprehensive database, RHRC researcher and statistical lead Julia Interrante is pulling data from multiple sources, such as the American Hospital Association’s surveys, a federal Provider of Services file, and information about hospital mergers and acquisitions. She and the team also rely on alerts from local news sources and cold calls to hospitals.

Because of these efforts, RHRC researchers know that in 2004, 45 percent of rural counties had no obstetric care. Fourteen years later, that number had risen to 56 percent. The RHRC first became aware of this issue in 2016 due to the observations of several grandmothers in a predominantly Black community in rural Alabama who noticed that pregnant people in their community were having to drive further away for obstetric care. They expressed concern to their congresswoman whose staff connected with federal rural health experts, who put in a call to Kozhimannil.
“We immediately changed the research program we had planned to answer the question that these rural grandmothers were asking,” said Kozhimannil. “We found that these grandmas were exactly right. Communities like theirs, rural communities with a higher proportion of Black residents, were more likely to lose maternity care.” This work fed into the 2018 Improving Access to Maternity Care Act, which passed Congress unanimously, to lay the groundwork for understanding how to address rural maternity care access and equity challenges.
In 2022, the White House laid out a plan to continue these efforts in the White House Blueprint for Addressing the Maternal Health Crisis, which heavily cites the team’s research. And in early April 2024, a bipartisan group of US senators, including Minnesota’s Tina Smith, introduced the Rural Obstetrics Readiness Act. Further inspired by RHRC’s research, the legislation aims to provide support to the many non-obstetric rural hospitals that must be prepared to provide potentially life-saving care to the people in labor that will inevitably show up at their doors when there isn’t time drive further to a hospital that does provide obstetric care.
This question posed by rural Alabama grandmothers has resulted in more than 25 studies published by RHRC researchers and a fuller understanding of the causes and effects of these closures, which is a problem across the United States but highly concentrated in more remote rural communities and rural communities with a high proportion of Black and Indigenous residents. Causes of these closures include clinical workforce shortages in obstetrics, family medicine, midwifery, and nursing, and clinicians sometimes lacking the necessary training, tools, or administrative support. Many physicians and nurses in these areas also don’t get the necessary training or experience to be able to handle more complicated births in rural settings. Medicaid also pays less for childbirth services than private insurance, and rural areas are more likely to have more births financed by Medicaid, creating a financial strain on rural hospitals in low-population communities with many Medicaid-funded births.

And the effects? Higher rates of preterm births, higher rates of births outside of hospitals, and higher rates of births in hospital emergency rooms. There is also data indicating an increased risk of complications associated with greater travel distance to access pregnancy and birth-related care. Rural residents in areas without obstetric care also have less access to other maternity support services, including childbirth education classes, breastfeeding and postpartum support, and doula care.
Other Factors at Play: Less Access to Midwifery Care and Higher Incidence of Intimate Partner Violence in Rural Communities
The RHRC is currently conducting research on rural access to midwifery care. The midwifery model tends to be person-centered and low intervention and has been shown to positively impact people’s pregnancies and births. It is also a model that’s preferred by many birthing people and can be associated with cost savings for low-risk hospital births.

“From a high level, we found that the majority of rural communities do not have locally available midwifery care. Hospitals in what we might consider to be medically underserved or vulnerable rural communities were more likely to lack local access to midwifery care, such as rural communities that are more remote or those with a majority population that identifies as Black, Indigenous, or People of Color,” said RHRC research assistant and second year PhD student Emily Sheffield, who is leading a paper on this topic.
RHRC researchers including Research & Policy Fellow Alyssa Fritz are also studying intimate partner violence (IPV) in rural communities. IPV is a significant contributor to maternal mortality, with homicide (frequently perpetrated by an intimate partner) being a leading non-obstetric cause of maternal deaths. The RHRC just wrapped up a project looking at rural-urban differences in IPV, and found that IPV is more prevalent among rural birthing people, who were less likely to be screened for abuse by a health care provider before, during, and after pregnancy than urban birthing people. Fritz interviewed direct service and advocacy organizations that support rural IPV victims and found that access to crisis centers is harder for folks in rural areas, local health care professionals and law enforcement may not have the necessary sexual or domestic assault training, and limited housing may force birthing people to stay with abusive partners if there are no other places to go.
According to Kozhimannil, structural urbanism plays a role in these issues. Academic health centers are based in urban communities. Almost all physicians train in urban areas. While some of them may have rural rotations, there is an urban bias to the resources, training, and support as well as the evidence base for medicine, public health, and health policy.
Rural Healthcare Facilities Celebrate Childbirth
Yet rural communities have a lot to offer birthing people. “I don’t want us to continue this discussion about how rural areas are so sad and a terrible place to give birth because they’re a wonderful place to give birth,” said Kozhimannil. “Birth is not just a medical experience, and many people working in rural healthcare facilities tend to treat childbirth like the cultural and family event that it is.”

RHRC has published a series of case studies called Making it Work, which depict successful models of rural maternity care. One shining example is Western Wisconsin Health in Baldwin, Wisconsin, a critical access hospital where even the physicians provide midwifery models of care with a focus on offering low intervention options for rural folks, including vaginal birth after Cesarean delivery. Rural Alaska’s Maniilaq Health Center, a tribal health facility that incorporates culturally-centered obstetric care for Alaska Native people, provides another example. The Maniilaq Case Study was led by Hailey Baker, a University of Minnesota-Duluth medical student and enrolled citizen of the Cherokee Nation, highlighting the RHRC’s commitment to cross-disciplinary and student-led research.
In addition to emphasizing the benefits of childbirth in rural communities, Kozhimannil also noted the harm caused by the term “maternity care desert.”
“The term ‘desert’ is often used to imply a wasteland, which isn’t true. Deserts are naturally occurring vibrant ecosystems and can be beautiful, flourishing climates where Indigenous people have survived for years and years, but places without maternity care are not naturally occurring, and they are not wastelands. Calling rural communities ‘maternity care deserts’ is not a rural-informed or land-based perspective,” Kozhimannil said. “Instead of saying ‘maternity care desert,’ say ‘places without maternity care.’ It’s just one more word.”